Aims of the TRAJECT Project
The central aim of the TRAJECT project is to better understand the different ways older people with serious chronic illnesses experience the last months of life. We are exploring whether there are common patterns —so-called trajectories— in how health and well-being change over time, and whether certain groups of people (for example, those with similar diagnoses or living in similar social conditions) tend to follow similar end-of-life trajectories.
At the same time, we want to understand the limits of these general patterns. Not every experience can —or should— be generalised. That’s why we also want to learn about the unique, individual aspects of each person’s end-of-life trajectory.
By identifying both shared patterns and personal variations, TRAJECT aims to generate crucial scientific insights that can help improve how we assess older people's needs and how we organise and deliver their care towards the end of life.

Objective 1
What are the different temporal patterns of physical, social, psychological, and existential well-being that older people with serious chronic illness experience towards the end of life, and how are these patterns connected to their personal, medical, and social characteristics?
Objective 2
What are the common themes, the differences, and changes in the narratives of older people’s health and well-being as they approach the end of life?
Objective 3
What can be learned by combining these patterns of well-being and the narratives in a mixed-method approach to better clarify both shared experiences and unique differences of older people approaching the end of life?
Study design
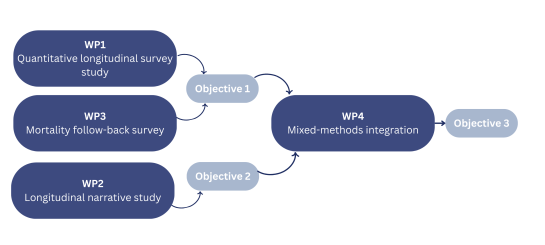
This project deploys a convergent mixed-methods study including a quantitative longitudinal survey study, a qualitative serial narrative study, and a quantitative mortality follow-back survey. Finally, all results will be integrated through triangulation and by systematically treading keys findings from one study to the next.
The infographic on the right shows how the objectives and methods relate to each other. See below for more detailed information on the methods/studies.
Methods
WORK PACKAGE 1:
A quantitative longitudinal study will involve 280 people aged 70 years or over and diagnosed with at least one serious chronic illness, each completing surveys every two months over the course of one year or shorter, if the participant dies before. The research aims to track and analyse the participants’ health and well-being trajectories in the physical, psychological, social and existential domains.
WORK PACKAGE 2:
A serial narrative interview study will be conducted with a smaller group of 30 participants, who also participate in the quantitative study. They will be invited to semi-structured narrative interviews, every two months over the course of one year or shorter, if the participant dies before. This study views end-of-life trajectories primarily as individual stories and, through them, explores the unique, subjective experiences of older adults with chronic illness.
WORK PACKAGE 3:
Upon the death of a participant, a close family member or caregiver will be invited to take part in a mortality follow-back survey to gather insights retrospectively into the last three months of the participant’s life, focusing on symptoms and concerns, health care utilisation, and aspects of communication among patient, family and healthcare providers. This survey will be conducted at least three months after the participant’s death. In addition to the survey, an open conversation will take place, allowing the family member to share their experience of the participant's final phase of life.
WORK PACKAGE 4:
Finally, we will weave together the mixed-methods findings from the three previous work packages. We will do this by triangulating the different findings and through a method called following-a-thread, whereby key findings from one study/method are followed through to the other methods/studies to investigate whether and in which form they appear there. This mixed methods integration will achieve a deep and comprehensive understanding of the end-of-life trajectories of older people with chronic illness.
