Aims & objectives
The central aim of the TRAJECT project is to find out what is general and what is unique in older people's end-of-life experiences and the circumstances that shape them. This means rethinking the way we have been studying health trajectories and factors shaping them. This requires a new approach that recognizes both the common experiences shared by many people and the unique aspects of each individual’s journey. We should treat differences as valuable information, especially when looking at well-being and all the factors that contribute to health in the final stages of life.
The findings will offer insights into the medical, social, and emotional factors that impact well-being at the end of life. This will help healthcare providers better meet the needs of different groups of patients, improving care and ensuring comfort and dignity in their final stages of life.

Objective 1
What are the different temporal patterns of physical, social, psychological, and existential well-being that older people with serious chronic illness experience towards the end of life, and how are these patterns connected to their personal, medical, and social characteristics?
Objective 2
What are the common themes, the differences, and changes in the narratives of older people’s health and well-being as they approach the end of life?
Objective 3
What can be learned by combining these patterns of well-being and the narratives in a mixed-method approach to better clarify both shared experiences and unique differences of older people approaching the end of life?
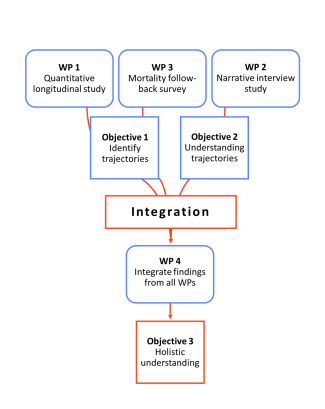
We intend to achieve the central aim of finding what is common and unique in older people’s end of life trajectories through multiple objectives outlined below (see diagram):
For the first objective, we use structured surveys (WP1) to discover what is common among the participants. However, we must acknowledge that beyond these common patterns, there are very personal experiences that surveys alone cannot capture. To truly understand these experiences, we need to genuinely listen to the participants. This is precisely what we will do in the second work package. When people talk about important health issues, like living with a chronic illness, they often do so by telling stories. In these open conversations we have with the participants, we do not expect them to just give a list of medical facts, but we give them room to tell us what happened and how they experienced these health issues. Furthermore, we will ask a family member or a close caregiver to share their thoughts and experiences about the health and well-being of the participant (WP3). With this approach we will have several perspectives on the health trajectory of the participant and the different circumstances that have shaped it.
By having this many participants, we will be able to see if there are similarities and which experiences can be shared when dealing with chronic illnesses. At the same time, by listening to their stories, we can learn about the unique and personal experience of each person. We will explore all the social, medical, psychological, and societal factors that shape their experiences and affect the health and well-being of older people.
All these findings and objectives will be combined (WP4), so we can make inferences on the experiences and changes health and well-being that older people in deteriorating health go through. This work will completely change how we look at older people living with chronic illness and their health trajectories. We know that there are a great many different factors that make up the experience of older people and that they are intertwined with one another. Nevertheless, by deploying different methods simultaneously, we can unravel the complexity of individual experiences and just as well discover common patterns.
Methods
To understand the end of life journeys of older people with chronic illness who are in deteriorating health, we combine quantitative and qualitative methods in a mixed-method study consisting of four work packages (see diagram). The first work package (WP1) is a quantitative longitudinal large-scale study making use of standardised questionnaires. We want to include 280 participants in WP1 and follow them up for one year. The study is longitudinal as each participant will complete the survey seven times. By following the participants for one year, we will be able to see if there are groups of participants who follow similar paths in their end of life journeys.
For the second work package (WP2), we will select a group of participants from WP1 and invite them to also voluntarily take part in the qualitative study. Over the course of a year, these participants, along with the seven quantitative assessments, will participate in open ended conversations about how they perceive and manage their illness. These conversations will give us an insight into the different end of life trajectories that people go through, and their unique experiences associated with it.
The third work package (WP3) builds further on WP1. On an unfortunate passing of the participant, we will invite a close family member or caregiver to participate in a survey about the last period of the participant’s life. To avoid adding to their grief, we will only conduct this survey at least three months after the participant's passing. The survey will be completed either in person or via telephone, and we will also have an open conversation about this period, where the family member can share their experiences and emotions.
Finally, all the results will be brought together in the last work package (WP4). Here, we will compare important findings from every work package, to understand what is different and similar in participants’ experiences at the end of life and why. The final goal of the study is to gain a holistic understanding of the end-of-life trajectories of older people with chronic illness.

Timeline of study participation
WP 1
Every two months, a researcher visits the participant at a location of their choice, usually their home, to complete a survey together. The participant does not need to write anything down, and the visit lasts about 45 minutes to an hour. Over the course of a year, there will be seven of these visits.
WP 2
For participants also taking part in the narrative study, there will be additional appointments between the survey visits to have an open conversation about their experience. The length of these conversations is entirely up to the participant. Like the surveys, there will be seven appointments spread over the year.
WP 3
On an unfortunate passing of the participant, the researcher will carry on conversation with a family member by phone or in person to learn more about the last months of the participant’s life. To avoid adding to their grief, this will only be done at least three months after the participant's passing.
Impact
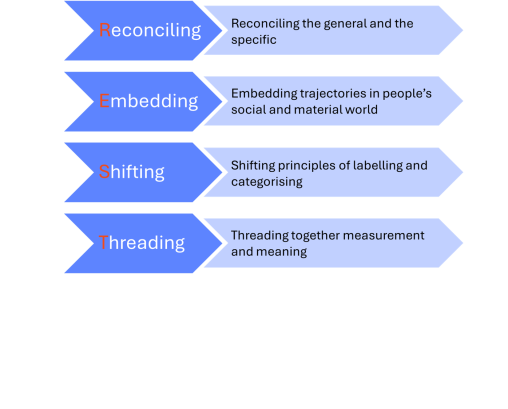
This study will help us better understand what it means to have a "good death". By exploring new perspectives, the goal is to improve how we care for people as they age and approach the end of life. The project focuses on uniting the common experiences we all share with the deeply personal aspects of each person's journey. It is based on the principles of REST: reconciling, embedding, shifting and threading.
Instead of just looking at medical factors, the project will examine how people’s social and physical environments affect their end-of-life experiences. This will help move beyond broad labels and generalisations, allowing us to focus on the individuality of each journey. We will also combine objectively measurable aspects of life with the personal meanings people attach to their experiences, giving us a fuller picture.
The findings will offer insights into the medical, social, and emotional factors that impact well-being at the end of life. This will help healthcare providers better meet the needs of different groups of patients, improving care and ensuring comfort and dignity in their final stages of life.
